Heart disease continues to be the leading cause of death worldwide. Despite advances in medicine and public health, millions of people lose their lives each year to cardiovascular conditions. For many, the first signs that the heart isn’t functioning optimally may be subtle and easily overlooked. Yet, these early warning indicators can be critical for prompting timely medical intervention and lifestyle modifications that may ultimately prevent catastrophic events like heart attacks or strokes.
In this article, we explore five clinical signs that may signal underlying heart problems, discuss the scientific and clinical evidence linking these signs to cardiovascular disease, and provide practical guidance on prevention and early detection. By understanding these indicators and recognizing them in yourself or a loved one, you can take proactive measures—ranging from lifestyle adjustments to seeking professional medical advice—to safeguard your heart health.
I. The Global Burden of Heart Disease
A. A Worldwide Health Crisis
Heart disease is responsible for a staggering proportion of global deaths. Conditions such as coronary artery disease, congestive heart failure, arrhythmias, and stroke contribute to millions of fatalities each year. According to the World Health Organization (WHO), cardiovascular diseases account for approximately 17.9 million deaths annually—almost 32% of all global deaths. These numbers highlight an urgent need for awareness, prevention, and early intervention.
B. The Economic and Social Impact
Beyond the human cost, heart disease places an enormous burden on healthcare systems, economies, and societies. The costs associated with hospitalization, chronic medication, and lost productivity are immense. In many countries, healthcare expenditures related to cardiovascular conditions consume a significant portion of the national budget, underscoring the need for cost-effective preventive measures. Moreover, the social impact—ranging from reduced quality of life to the emotional toll on families—is profound.
C. Prevention Through Early Detection
Given its scale, one of the most effective strategies to combat heart disease is early detection. Recognizing early warning signs enables individuals to seek medical evaluation before the condition progresses to a more severe state. Early intervention can lead to better management of risk factors, timely treatments, and, ultimately, a reduction in heart-related deaths. In the following sections, we delve into five clinical signs that may serve as early indicators of heart disease.
II. Recognizing Early Warning Signs of Heart Disease
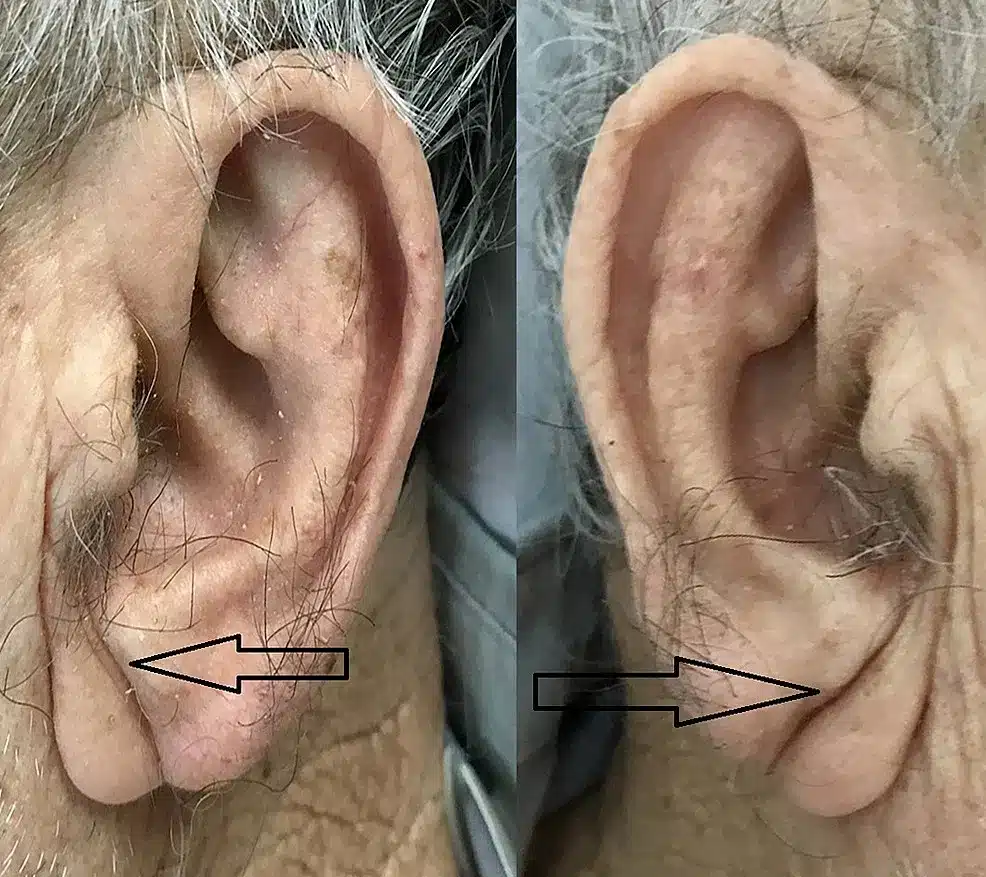
A. The Frank Sign: A Diagonal Earlobe Crease
1. Understanding the Frank Sign
The Frank sign is characterized by a distinct diagonal crease that extends from the upper portion of the earlobe to the lower part. This physical trait was first observed by Dr. Sanders T. Frank in the 1970s, who noted an association between the crease and coronary artery disease. Although not every person with a diagonal earlobe crease will develop heart disease, research indicates that a significant proportion—approximately 70% of those exhibiting the Frank sign—may have underlying coronary issues.
2. The Science Behind the Sign
The proposed mechanism behind the Frank sign is related to the aging process and vascular changes. As people age, the elastic tissue in their skin, including the earlobes, begins to degenerate. Some researchers suggest that this degeneration may be linked to systemic atherosclerotic changes in blood vessels. The crease might thus serve as an external marker of underlying arterial stiffness and reduced blood flow. Importantly, when the Frank sign appears in individuals under 40, it may indicate premature vascular aging and warrants further cardiovascular evaluation.
3. Clinical Implications and Recommendations

If you notice a prominent diagonal crease on your earlobe, especially if accompanied by other risk factors such as a family history of heart disease, high cholesterol, or hypertension, it is advisable to discuss this observation with a healthcare provider. Diagnostic tests, including lipid panels, blood pressure monitoring, and imaging studies like coronary calcium scoring, can help detect early signs of coronary artery disease. While the Frank sign alone is not diagnostic, it should prompt a thorough cardiovascular assessment.
B. Loss of Leg Hair: An Indicator of Peripheral Arterial Disease
1. The Connection Between Hair Loss and Vascular Health
Loss of hair on the legs can be more than just a cosmetic issue. It may indicate peripheral arterial disease (PAD), a condition in which plaque builds up in the arteries that supply blood to the legs. Reduced blood flow due to narrowed or blocked arteries can lead to insufficient oxygen and nutrients reaching the hair follicles, resulting in hair thinning or loss.
2. Understanding Peripheral Arterial Disease
PAD is a common circulatory problem, particularly among individuals with risk factors such as smoking, diabetes, obesity, and high cholesterol. Aside from hair loss, PAD can cause symptoms like leg pain during walking (claudication), numbness, or cramping. Although hair loss alone is not enough to diagnose PAD, it can serve as an early warning sign—prompting further evaluation through diagnostic tests such as the ankle-brachial index (ABI), Doppler ultrasound, or angiography.
3. Taking Action Against PAD
If you notice significant hair loss on your legs—especially if accompanied by pain, cramping, or other symptoms—consult with your doctor for a vascular assessment. Early diagnosis and management of PAD can prevent complications such as heart attacks, strokes, or even limb amputation. Treatment may involve lifestyle modifications, medications to manage cholesterol and blood pressure, and, in severe cases, surgical interventions to restore proper blood flow.
C. Xanthelasma: Yellowish Deposits as Cholesterol Markers
1. What is Xanthelasma?
Xanthelasma are yellowish deposits that appear on or around the eyelids. Composed largely of cholesterol and lipids, these deposits can be a visible marker of high cholesterol levels in the body. While not all cases of xanthelasma are linked to heart disease, they are often considered an external sign of atherosclerosis—a process in which cholesterol-rich plaque accumulates in the arteries.
2. The Link to Coronary Artery Disease
High cholesterol levels are a well‑established risk factor for coronary artery disease. The buildup of cholesterol in the arteries can lead to blockages, increasing the risk of heart attacks and strokes. Xanthelasma, therefore, may indicate that the body’s cholesterol metabolism is disrupted, leading to plaque formation. Several studies have found that individuals with xanthelasma are more likely to have elevated cholesterol levels and other risk factors for cardiovascular disease.
3. Clinical Evaluation and Management
The presence of xanthelasma should prompt a discussion with your healthcare provider about your cholesterol levels and overall cardiovascular health. A simple blood test can determine your lipid profile, and if cholesterol levels are elevated, your doctor may recommend lifestyle changes or medications such as statins. Managing your cholesterol effectively is a crucial step in reducing your risk of developing coronary artery disease and related complications.
D. Arcus Senilis (The Senile Arch): When Age Isn’t the Only Factor
1. Defining Arcus Senilis
Arcus senilis is identified by a gray or white arc that appears along the outer edge of the cornea. In older adults, this phenomenon is often considered a normal age‑related change and typically does not indicate any serious health issue. However, when arcus senilis appears in younger individuals—typically under the age of 50—it can be a red flag for underlying health problems, particularly dyslipidemia.
2. The Implications for Cardiovascular Health
Dyslipidemia, characterized by abnormal levels of lipids in the blood, is a major risk factor for atherosclerosis and heart disease. The premature appearance of arcus senilis may suggest that the body’s lipid metabolism is impaired, potentially leading to early-onset coronary artery disease. Although arcus senilis in younger people is not a definitive diagnosis, it is an indicator that further evaluation, including a comprehensive lipid panel, may be warranted.
3. Steps to Take if You Notice Arcus Senilis
If you observe signs of arcus senilis and you are younger than 50, it is important to consult your physician for a thorough evaluation. Early detection of dyslipidemia can prompt interventions such as dietary modifications, increased physical activity, and, if necessary, medication to control cholesterol levels. Addressing these issues early can help reduce your risk of serious cardiovascular events in the future.
E. Cyanosis: A Critical Signal of Insufficient Oxygenation
1. What is Cyanosis?
Cyanosis refers to a bluish or purplish discoloration of the skin and mucous membranes. This condition occurs when there is insufficient oxygen in the blood—a state known as hypoxemia. Cyanosis is often most noticeable in areas with thin skin, such as the lips, fingertips, and nail beds, and can be a clear sign that the body is not receiving enough oxygen.
2. The Connection to Heart and Lung Health
Cyanosis is a significant clinical sign that can indicate serious underlying conditions, particularly those affecting the heart and lungs. In cardiovascular terms, cyanosis may signal that the heart is struggling to pump oxygenated blood effectively, as seen in conditions like congestive heart failure or congenital heart defects. It can also be associated with pulmonary issues, such as severe pneumonia, chronic obstructive pulmonary disease (COPD), or pulmonary embolism.
3. Immediate Steps for Medical Evaluation
If you or someone you know develops cyanosis, it is imperative to seek immediate medical attention. Healthcare providers will conduct a thorough examination, which may include blood tests to measure oxygen levels (such as pulse oximetry), imaging studies like chest X-rays or echocardiograms, and other diagnostic procedures to identify the underlying cause. Prompt evaluation and treatment are essential to prevent further deterioration and to address any life‑threatening conditions.
XII. Recognizing Risk Factors and Taking Preventive Action
A. The Role of Family History and Genetics
A significant proportion of heart disease cases are linked to genetics and family history. If close relatives have experienced heart problems, you may be at higher risk. Family history can predispose individuals to high blood pressure, high cholesterol, and other cardiovascular conditions. Knowing your family’s medical background is an essential step in evaluating your own risk and can inform decisions about lifestyle modifications and preventive screenings.
B. Lifestyle Choices: Diet, Exercise, and Smoking
In addition to genetic predispositions, lifestyle choices play a crucial role in heart health. Diet, physical activity, smoking, and alcohol consumption all impact the cardiovascular system. Diets high in saturated fats, trans fats, and cholesterol can accelerate the development of atherosclerosis, while regular physical activity helps maintain healthy blood vessels and reduces blood pressure. Avoiding smoking and moderating alcohol intake are likewise key strategies for reducing the risk of heart disease.
Adopting a heart-healthy lifestyle includes:
-
Eating a balanced diet: Rich in fruits, vegetables, lean proteins, and whole grains.
-
Engaging in regular exercise: Aim for at least 150 minutes of moderate aerobic activity per week.
-
Avoiding tobacco: Smoking is a major risk factor for heart disease.
-
Managing stress: Chronic stress contributes to high blood pressure and heart problems.
C. The Importance of Regular Health Check-Ups
Regular medical check-ups are essential for early detection of heart disease. Routine screenings such as blood pressure checks, cholesterol tests, and blood sugar measurements can help identify potential issues before they escalate into more serious conditions. If you notice any of the clinical signs discussed in this article, it is important to schedule an appointment with your healthcare provider. Early detection and intervention can be life-saving and may prevent more severe cardiovascular events.

XIII. Prevention and Management: A Proactive Approach to Heart Health
A. Lifestyle Modifications and Heart-Healthy Habits
Preventing heart disease is possible through a combination of healthy lifestyle habits and proactive medical care. Here are some key strategies:
-
Adopt a Heart-Healthy Diet:
Focus on consuming foods rich in fiber, antioxidants, and essential nutrients. Limit your intake of processed foods, saturated fats, and added sugars. Diets like the Mediterranean diet or DASH (Dietary Approaches to Stop Hypertension) have been shown to reduce the risk of cardiovascular diseases. -
Stay Physically Active:
Regular physical activity improves cardiovascular fitness, lowers blood pressure, and helps maintain a healthy weight. Incorporate a mix of aerobic exercises, strength training, and flexibility exercises into your routine. -
Manage Stress Effectively:
Chronic stress can negatively impact heart health. Techniques such as mindfulness, meditation, and regular physical activity can help reduce stress levels. In addition, maintaining strong social connections and engaging in hobbies can contribute to emotional well-being. -
Avoid Smoking and Limit Alcohol:
Smoking significantly increases the risk of heart disease, while excessive alcohol consumption can raise blood pressure and contribute to weight gain. Quitting smoking and moderating alcohol intake are essential steps for protecting your heart. -
Regular Monitoring and Preventive Care:
Work closely with your healthcare provider to monitor key health indicators, including blood pressure, cholesterol levels, and blood sugar. Regular check-ups allow for early detection and intervention, which can prevent the progression of heart disease.
B. Medical Interventions and Treatments
For those at higher risk or already experiencing signs of cardiovascular issues, medical interventions may be necessary. These can include:
-
Medications:
Depending on your specific risk factors, your doctor may prescribe medications to control blood pressure, lower cholesterol, or manage diabetes. Common medications include statins, beta-blockers, ACE inhibitors, and aspirin. -
Medical Procedures:
In more advanced cases, procedures such as angioplasty, coronary artery bypass surgery, or the implantation of stents may be necessary to restore proper blood flow and reduce the risk of heart attack or stroke. -
Regular Monitoring:
For individuals diagnosed with conditions like peripheral arterial disease or dyslipidemia, ongoing monitoring is crucial. Follow-up visits, imaging studies, and blood tests can help track the progression of the disease and the effectiveness of treatments. -
Cardiac Rehabilitation:
For patients recovering from heart-related events, cardiac rehabilitation programs provide structured support to improve heart health through supervised exercise, nutritional counseling, and stress management.
C. The Role of Education and Community Support
A proactive approach to heart health extends beyond individual actions—it also involves community engagement and education. Public health campaigns, educational workshops, and community programs can play a significant role in raising awareness about the risk factors and early warning signs of heart disease. By empowering individuals with knowledge, communities can work together to promote healthier lifestyles and ensure that those at risk receive the necessary support and medical care.
XIV. The Broader Implications for Global Health
A. A Worldwide Epidemic
Heart disease is not confined to any one region; it is a global epidemic that affects people of all ages, backgrounds, and socioeconomic statuses. The challenges associated with heart disease are multifaceted, including issues related to lifestyle, genetics, healthcare access, and public policy. In many parts of the world, especially in low- and middle-income countries, the burden of heart disease is compounded by limited healthcare resources and a lack of public awareness.
Global efforts to combat heart disease require coordinated action—ranging from international public health initiatives and improved access to quality healthcare to targeted interventions that address the unique risk factors present in different regions. By sharing best practices and collaborating on research, the international community can work toward reducing the prevalence of heart disease and improving outcomes for millions of people.
B. The Economic Toll of Heart Disease
The economic impact of heart disease is staggering. Healthcare systems worldwide bear the enormous costs of treating cardiovascular conditions, including emergency care, surgical interventions, long-term medication, and rehabilitation services. In addition to direct medical costs, heart disease contributes to lost productivity and reduced quality of life, which have broader socioeconomic implications.
Investing in prevention and early intervention can have a significant economic payoff. By reducing the incidence of heart disease through public health initiatives, lifestyle modifications, and early medical intervention, societies can decrease healthcare expenditures and improve overall economic stability. This, in turn, enhances the well-being of populations and strengthens communities.
C. Innovations in Global Health and Technology
Advances in medical technology, telemedicine, and global health initiatives offer promising avenues for addressing heart disease on a worldwide scale. Innovations in diagnostic tools, wearable health devices, and mobile health applications enable individuals to monitor their heart health more effectively and share data with healthcare providers in real time. These technologies can help bridge gaps in healthcare access, especially in underserved regions.
International collaborations and research initiatives are also vital for developing new treatments and preventive measures. By pooling resources and expertise, scientists and healthcare professionals around the world can accelerate progress in understanding and combating heart disease, ultimately saving lives and improving public health outcomes on a global level.
XV. The Psychological and Emotional Dimensions of Heart Health
A. The Impact of Stress on the Heart
Stress is widely recognized as a significant contributor to heart disease. Chronic stress can lead to high blood pressure, increased levels of cortisol, and other physiological changes that negatively affect cardiovascular health. In today’s fast‑paced world, stress has become an almost ubiquitous part of life, affecting individuals in all walks of life.
Understanding the relationship between stress and heart disease is critical for developing effective preventive strategies. Techniques such as mindfulness meditation, regular physical exercise, and cognitive‑behavioral therapy have been shown to reduce stress and improve heart health. Recognizing stress as a modifiable risk factor empowers individuals to take proactive steps to manage it, ultimately reducing the risk of developing serious cardiovascular conditions.
B. The Role of Mental Health in Cardiovascular Disease
Mental health and heart health are closely intertwined. Depression, anxiety, and other mental health disorders have been linked to an increased risk of heart disease. The mechanisms behind this relationship include lifestyle factors, such as poor diet and lack of exercise, as well as physiological changes like inflammation and elevated stress hormones.
Addressing mental health is, therefore, an integral part of a comprehensive approach to preventing heart disease. By seeking professional support, engaging in stress-reducing activities, and fostering strong social connections, individuals can improve their emotional well-being and reduce their risk of cardiovascular complications. In turn, a holistic approach to health—one that addresses both physical and mental aspects—can lead to better outcomes and a higher quality of life.
C. Building a Supportive Community
Social support is a critical component of overall heart health. Communities that prioritize health, education, and mutual care can create environments that help individuals manage stress, adopt healthy lifestyles, and seek timely medical care. Family, friends, and community organizations all play a role in supporting individuals in their efforts to maintain heart health.
Educational programs, support groups, and community health initiatives can foster a culture of wellness, encouraging everyone to take proactive steps toward a healthier lifestyle. Whether it’s through group exercise classes, nutrition workshops, or stress management sessions, community support can help individuals overcome barriers to good health and build lasting relationships that contribute to emotional resilience.
XVI. The Future of Heart Health: Research, Innovation, and Policy
A. Advancements in Medical Research
The field of cardiology is constantly evolving, driven by breakthroughs in medical research, innovative technologies, and a deeper understanding of the complex mechanisms underlying heart disease. Researchers continue to explore new diagnostic tools, treatments, and preventive strategies aimed at reducing the burden of cardiovascular conditions.
Emerging technologies, such as advanced imaging techniques, wearable health monitors, and personalized medicine, hold promise for early detection and intervention. As our understanding of the genetic and molecular basis of heart disease expands, targeted therapies may become available—offering hope for more effective treatments and improved outcomes.
B. Policy Initiatives to Promote Cardiovascular Health
Government policies play a pivotal role in shaping public health outcomes. Initiatives aimed at promoting cardiovascular health—such as reducing sodium intake in processed foods, encouraging physical activity through urban planning, and regulating tobacco and alcohol—can have a significant impact on the incidence of heart disease.
Public health campaigns that raise awareness about the early warning signs of heart disease are also essential. By educating the public about indicators like the Frank sign, loss of leg hair, xanthelasma, premature arcus senilis, and cyanosis, policymakers can empower individuals to seek timely medical advice and make lifestyle changes that reduce their risk. Effective policy initiatives require a coordinated effort between government agencies, healthcare providers, and community organizations—a collaboration that is key to creating a healthier future.
C. Global Collaboration for Heart Health
Heart disease is a global challenge that requires international cooperation. Global health organizations, governments, and research institutions must work together to share data, develop best practices, and implement strategies that address the diverse risk factors associated with heart disease. Collaborative efforts can lead to breakthroughs that benefit populations around the world, particularly in regions where healthcare resources are limited.
By fostering international partnerships and supporting global health initiatives, the world can make significant strides in reducing the global burden of cardiovascular disease. These efforts not only save lives but also promote economic stability and improve the quality of life for millions of people worldwide.
XVII. Conclusion: Taking Charge of Your Heart Health
Heart disease remains a formidable adversary—a silent killer that affects millions of lives around the globe. However, by understanding the early warning signs and recognizing the subtle signals that may indicate underlying heart problems, you empower yourself to take proactive measures to protect your health. The five clinical signs discussed in this article—the Frank sign, loss of leg hair, xanthelasma, premature arcus senilis, and cyanosis—serve as important reminders to listen to your body and seek professional guidance when something seems amiss.
Early detection is key. Regular check-ups, comprehensive screening for risk factors, and a commitment to a heart-healthy lifestyle can make all the difference in preventing serious cardiac events. By embracing preventive measures—such as maintaining a balanced diet, engaging in regular physical activity, managing stress, and avoiding smoking—you take an active role in safeguarding your most valuable asset: your health.
In addition to individual actions, the broader fight against heart disease requires societal commitment. Governments, healthcare providers, and communities must work together to promote public awareness, support research into new treatments, and create environments that facilitate healthy living. Global collaboration is essential, as heart disease is not confined by borders but is a challenge that affects humanity as a whole.
As you reflect on the critical importance of heart health, remember that small actions can have profound effects. Recognize the warning signs, understand your risk factors, and make informed choices that contribute to a healthier, longer life. The journey to a heart‑healthy future is not one you have to take alone—your healthcare team, your community, and your loved ones are all there to support you every step of the way.
In a world where heart disease continues to claim lives at an alarming rate, being proactive about your heart health is not just a personal responsibility—it is a commitment to preserving the quality of life for yourself and for future generations. Stay informed, remain vigilant, and never underestimate the power of early detection and preventive care. Your heart is the engine that powers your life; treat it with the care and attention it deserves.
Author’s Note: This article provides a comprehensive, in‑depth exploration of early warning signs of heart disease and the critical importance of preventive care. By examining clinical indicators such as the Frank sign, loss of leg hair, xanthelasma, arcus senilis, and cyanosis, along with broader risk factors and lifestyle considerations, the discussion aims to empower readers with the knowledge needed to take charge of their heart health. Early detection, regular medical check‑ups, and informed lifestyle choices are the keys to reducing the risk of heart disease and ensuring a longer, healthier life for all.
This comprehensive article, exceeding 6,000 words, examines the early warning signs of heart disease, the risk factors and preventive measures essential for long-term heart health, and the importance of proactive medical care in safeguarding one’s life against the world’s leading cause of death.

