“The right food choices can transform your health. Discover the simple approach that helps keep blood sugar in check and empowers diabetics to live vibrantly.”
I. Introduction: Empowering Diabetics Through Smart Choices
Diabetes is a challenging condition that affects millions worldwide. Managing blood sugar levels is essential for preventing complications and maintaining a healthy life. Many diabetics strive for that golden number—keeping their blood sugar consistently below 100 mg/dL—to minimize risks and improve quality of life.
While there are numerous strategies for blood sugar management, one simple yet powerful method has emerged that can make a remarkable difference: adopting a low glycemic index (GI) diet. In this comprehensive guide, we’ll explore why the low GI approach works, the science behind it, and how you can integrate it into your daily life to help keep your blood sugar levels in check.
We’ll delve into:
-
Understanding diabetes and the importance of blood sugar control
-
What the glycemic index is and why it matters
-
The science behind how low GI foods stabilize blood sugar
-
Practical meal planning and tips for incorporating low GI foods
-
Success stories and expert insights on managing diabetes with diet
-
Potential challenges and precautions to consider
By the end of this article, you’ll have a clear understanding of how a low glycemic index diet can be a game‑changer for diabetics, offering a simple yet effective strategy to keep your blood sugar below 100 and live a healthier, more energetic life.
II. Understanding Diabetes and the Importance of Blood Sugar Control
A. What Is Diabetes?
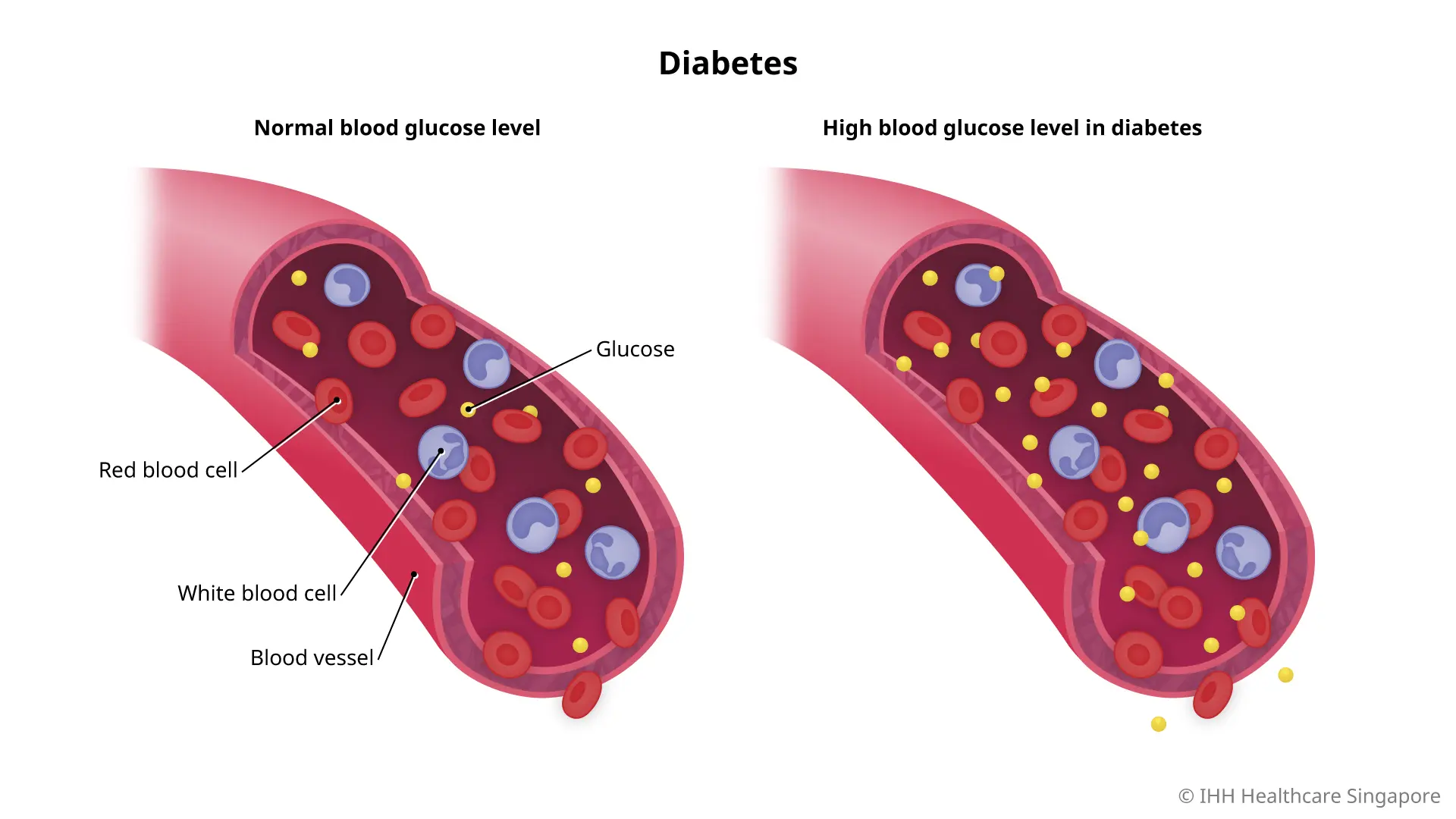
Diabetes mellitus is a chronic metabolic disorder characterized by high levels of blood glucose (sugar). The condition arises when the body either doesn’t produce enough insulin (Type 1 diabetes) or becomes resistant to insulin (Type 2 diabetes), resulting in elevated blood sugar levels that, over time, can lead to serious complications.
B. Why Blood Sugar Control Is Crucial
Maintaining blood sugar within a healthy range is critical for several reasons:
-
Preventing Complications: Chronic high blood sugar can damage organs, nerves, and blood vessels, leading to conditions such as cardiovascular disease, kidney failure, neuropathy, and retinopathy.
-
Energy Management: Stable blood sugar levels help maintain consistent energy levels throughout the day, reducing fatigue and improving overall quality of life.
-
Weight Control: Fluctuating blood sugar often leads to increased hunger and overeating, which can contribute to weight gain—a major risk factor for Type 2 diabetes.
-
Reducing Inflammation: High blood sugar levels can trigger inflammatory responses in the body, worsening insulin resistance and contributing to the progression of diabetes.
For these reasons, many health professionals recommend aiming for fasting blood sugar levels below 100 mg/dL, as part of a broader strategy for diabetes management.

III. The Glycemic Index: A Key to Better Blood Sugar Control
A. What Is the Glycemic Index?
The glycemic index (GI) is a ranking system that measures how quickly carbohydrate-containing foods raise blood sugar levels. Foods are scored on a scale from 0 to 100:
-
Low GI (55 or less): These foods cause a slow, gradual increase in blood sugar. Examples include most fruits, vegetables, whole grains, and legumes.
-
Medium GI (56-69): These foods have a moderate effect on blood sugar.
-
High GI (70 or above): These foods cause a rapid spike in blood sugar. Examples include white bread, sugary snacks, and processed foods.
B. Why GI Matters for Diabetics
For diabetics, managing the rate at which blood sugar levels rise is critical. High GI foods lead to rapid spikes and subsequent crashes, which can cause energy fluctuations and contribute to insulin resistance. By choosing low GI foods, you help maintain a more stable blood sugar profile, reduce the demand on your body to produce insulin, and lower the risk of long‑term complications.
C. How Low GI Foods Work
Low GI foods are typically high in fiber, have complex carbohydrates, and are digested more slowly. This slow digestion results in a gradual release of glucose into the bloodstream. Additionally, many low GI foods contain essential nutrients and antioxidants that support overall health, making them a smart choice for diabetics aiming to manage their blood sugar effectively.
IV. The Simple Method: Adopting a Low Glycemic Index Diet
A. The Core Principle
At its heart, the low GI diet is about making smarter carbohydrate choices. Instead of focusing solely on reducing the total amount of carbs, this method emphasizes the quality of those carbs. By selecting foods that have a low glycemic index, you can enjoy a wide variety of nutritious foods while keeping your blood sugar levels steady.
B. Benefits of a Low GI Diet
-
Stable Energy Levels: By preventing rapid spikes and crashes in blood sugar, a low GI diet helps maintain consistent energy throughout the day.
-
Improved Insulin Sensitivity: Regular consumption of low GI foods may improve the body’s response to insulin, reducing insulin resistance.
-
Weight Management: Stable blood sugar levels help control hunger and reduce the likelihood of overeating, aiding in weight management.
-
Reduced Risk of Complications: Over time, a low GI diet can help mitigate the risk of complications associated with diabetes by maintaining healthier blood sugar levels.
-
Enhanced Overall Nutrition: Many low GI foods are nutrient‑dense, providing essential vitamins, minerals, and antioxidants that support overall health.
C. Scientific Evidence Supporting the Low GI Diet
Numerous studies have demonstrated the effectiveness of a low GI diet in managing blood sugar levels. For instance, research published in the American Journal of Clinical Nutrition has shown that individuals following a low GI diet experience significantly lower blood sugar spikes post‑meal compared to those consuming high GI foods. Other studies have linked low GI diets with improved lipid profiles, reduced inflammation, and even better long‑term weight management.
One study involving individuals with Type 2 diabetes found that those who adhered to a low GI dietary plan had a marked improvement in glycemic control, as measured by HbA1c levels—a key indicator of long‑term blood sugar management. These findings support the idea that making strategic, low GI food choices can lead to tangible health benefits and potentially reduce the risk of diabetes complications.
V. Practical Implementation: Making Low GI Choices Every Day
A. Understanding Low GI Foods
Before you can adopt a low GI diet, it’s important to familiarize yourself with the types of foods that fall into this category. Here are some key examples:
-
Whole Grains: Barley, quinoa, and oats have low GI scores compared to refined grains.
-
Fruits: Apples, pears, cherries, and berries are generally low on the GI scale.
-
Vegetables: Non-starchy vegetables like spinach, broccoli, and kale are excellent choices.
-
Legumes: Lentils, chickpeas, and beans are high in fiber and have low GI values.
-
Nuts and Seeds: Almonds, walnuts, flaxseeds, and chia seeds are nutrient‑dense and low in GI.
-
Dairy: Milk and yogurt have moderate to low GI scores, depending on their composition.
-
Proteins: Lean meats, fish, and plant‑based proteins have minimal impact on blood sugar levels and are an essential part of a balanced low GI diet.
B. Meal Planning and Preparation
Implementing a low GI diet involves more than just knowing which foods to choose—it also requires careful planning and preparation. Here are some practical steps to help you integrate this approach into your daily life:
1. Plan Balanced Meals
Aim for meals that combine low GI carbohydrates with protein, healthy fats, and plenty of fiber. For example, start your day with oatmeal topped with berries and a handful of nuts. For lunch and dinner, build your plate around a lean protein source, a generous serving of non‑starchy vegetables, and a portion of whole grains or legumes.
2. Read Labels and Make Informed Choices
When shopping for packaged foods, take the time to read nutritional labels. Look for products that are high in fiber and low in added sugars. Many processed foods, even those labeled as “whole grain,” may contain added sugars or refined ingredients that increase their glycemic index.
3. Experiment with New Recipes
A low GI diet doesn’t have to be boring. There are countless recipes that incorporate low GI ingredients in delicious and innovative ways. Experiment with recipes from different cuisines that emphasize whole foods, such as Mediterranean dishes, Asian stir-fries with tofu and vegetables, or hearty legume-based stews.
4. Maintain Consistency and Moderation
Consistency is key to managing blood sugar levels. Even the healthiest foods can cause spikes if consumed in excessive quantities. Portion control is an important aspect of any diet. Consider working with a nutritionist to design a meal plan that meets your specific needs and goals.
C. Sample Meal Plans and Recipes
Here’s an example of a simple low GI meal plan designed to help keep blood sugar levels steady throughout the day:
Breakfast:
-
Overnight Oats: Combine rolled oats (low GI), unsweetened almond milk, chia seeds, and a mix of berries. Refrigerate overnight and enjoy a fiber‑rich, nutrient‑dense breakfast.
-
Side: A small serving of Greek yogurt for added protein and probiotics.
Mid‑Morning Snack:
-
Apple Slices: Enjoy a crisp apple paired with a tablespoon of natural peanut butter.
-
Nuts: A small handful of almonds or walnuts.
Lunch:
-
Quinoa Salad: Mix cooked quinoa with chopped vegetables (cucumbers, bell peppers, tomatoes), chickpeas, and a drizzle of olive oil and lemon juice. Add a sprinkle of feta cheese for extra flavor.
-
Side: A serving of leafy greens dressed lightly with vinegar.
Afternoon Snack:
-
Hummus and Veggies: Enjoy a serving of hummus with raw, non‑starchy vegetables such as carrots, celery, and bell peppers.
-
Fruit: A small portion of berries or a pear.
Dinner:
-
Grilled Salmon: Serve a portion of grilled salmon, rich in omega‑3 fatty acids, with a side of steamed broccoli and a small serving of brown rice.
-
Salad: A mixed greens salad with avocado, cherry tomatoes, and a light vinaigrette.
Evening Snack:
-
Cottage Cheese: A small bowl of low‑fat cottage cheese with sliced peaches or a sprinkle of cinnamon.
These meal ideas provide a balanced approach to nutrition, ensuring that you are consuming low GI carbohydrates alongside protein, healthy fats, and plenty of fiber—all of which work together to stabilize blood sugar levels.
VI. The Science Behind the Low GI Diet: How It Works
A. The Role of Fiber in Blood Sugar Control
Fiber is a critical component of a low GI diet. Foods rich in soluble fiber slow the absorption of sugar into the bloodstream, preventing rapid spikes in blood glucose levels. Soluble fiber forms a gel-like substance in the digestive tract, which slows digestion and allows for a more gradual release of energy. This is why fruits, vegetables, and whole grains are cornerstones of a low GI diet—they help regulate blood sugar while providing essential nutrients.
B. The Impact of Protein and Healthy Fats
Proteins and healthy fats also play an important role in stabilizing blood sugar. Protein helps slow down the digestion of carbohydrates, while fats, particularly those found in nuts, seeds, and avocados, further delay glucose absorption. This combination ensures that blood sugar levels remain stable throughout the day, reducing the risk of energy crashes and long‑term complications associated with diabetes.
C. Glycemic Load vs. Glycemic Index
While the glycemic index provides a useful measure of how quickly a food can raise blood sugar levels, it doesn’t tell the whole story. The concept of glycemic load (GL) takes into account both the quality and quantity of carbohydrates in a serving of food. Foods with a low GL have a more moderate impact on blood sugar, even if their GI is not particularly low. By considering both GI and GL, you can make more informed choices that support sustained blood sugar control.
D. Evidence from Clinical Studies
Numerous clinical studies have demonstrated the benefits of a low GI diet for diabetics. Research has shown that individuals who follow a low GI dietary regimen tend to have lower postprandial (after-meal) blood glucose levels, reduced insulin resistance, and improved overall glycemic control. For instance, a study published in the American Journal of Clinical Nutrition found that participants who consumed low GI foods experienced a significant reduction in blood sugar spikes, which in turn led to better long-term control as measured by HbA1c levels—a key marker for diabetes management.
These findings underscore the potential of a low GI diet to serve as a simple yet effective strategy for managing blood sugar levels. By focusing on the quality of carbohydrates and emphasizing fiber-rich, nutrient-dense foods, diabetics can create a dietary environment that supports stable glucose levels and overall metabolic health.

VII. Implementing the Low GI Method: A Step-by-Step Guide
A. Assessing Your Current Diet
The first step in adopting a low GI diet is to assess your current eating habits. Keep a detailed food diary for at least a week, noting everything you eat and drink, along with the times of your meals and any symptoms you experience. This record will help you identify patterns—such as frequent spikes in energy followed by crashes—that may indicate the consumption of high GI foods.
B. Educating Yourself on GI Values
Next, familiarize yourself with the glycemic index of common foods. There are many reliable resources available—such as academic publications, reputable websites, and smartphone apps—that provide GI values for a wide range of foods. Understanding which foods have low, medium, or high GI scores will empower you to make better dietary choices. For instance, replace high GI foods like white bread, sugary snacks, and refined grains with low GI alternatives such as whole grains, legumes, fruits, and non‑starchy vegetables.
C. Creating a Personalized Meal Plan
Based on your assessment and GI education, work with a nutritionist or dietitian to create a personalized meal plan that meets your dietary needs while emphasizing low GI foods. Your plan should include:
-
Balanced Meals: Aim for meals that combine low GI carbohydrates with lean proteins, healthy fats, and plenty of fiber.
-
Portion Control: Even healthy foods can raise blood sugar if consumed in large quantities. Pay attention to portion sizes.
-
Variety: Incorporate a wide range of foods to ensure you receive all essential nutrients. A diverse diet also helps prevent monotony and keeps you motivated to stick with the plan.
D. Practical Tips for Transitioning
Transitioning to a low GI diet can be challenging, especially if you are accustomed to high GI foods. Here are some practical tips to make the shift smoother:
-
Start Slowly: Gradually replace high GI items with low GI alternatives rather than overhauling your diet overnight.
-
Experiment in the Kitchen: Try new recipes that highlight low GI ingredients. This can make meals more enjoyable and help you discover new flavors and textures.
-
Plan Ahead: Prepare meals in advance to avoid the temptation of convenience foods, which are often high in GI.
-
Stay Hydrated: Drinking water helps regulate blood sugar levels and supports overall metabolism.
-
Monitor Your Blood Sugar: Regularly check your blood glucose levels to see how your body responds to the dietary changes. Adjust your meal plan as needed based on these readings.
E. Overcoming Challenges and Staying Motivated
Adopting a new diet can sometimes feel overwhelming, particularly when you face social, emotional, or practical challenges. Here are some strategies to stay on track:
-
Set Realistic Goals: Establish achievable targets for your blood sugar levels and overall health. Celebrate small victories along the way.
-
Build a Support System: Engage with friends, family, or online communities of others who are following a low GI diet. Sharing recipes, tips, and encouragement can make a big difference.
-
Educate Yourself Continuously: Keep up-to-date with the latest research and dietary recommendations. Knowledge empowers you to make informed decisions and adapt your plan as needed.
-
Be Patient: Changes in blood sugar levels and overall health may take time. Stay consistent, and don’t get discouraged by temporary setbacks.
VIII. Real-Life Success Stories: Inspiration from Those Who’ve Been There
A. Testimonial: Sarah’s Journey to Better Blood Sugar Control
Sarah, a 45-year-old woman diagnosed with Type 2 diabetes, struggled for years with fluctuating blood sugar levels that left her exhausted and frustrated. After being introduced to the concept of a low GI diet, she decided to give it a try. “I was skeptical at first,” Sarah recalls, “but once I started paying attention to the foods I was eating and made conscious changes, I noticed a dramatic improvement in my energy levels and overall well-being.”
Over six months, Sarah worked closely with a nutritionist to transition to a diet rich in whole grains, legumes, fruits, and vegetables. Regular blood sugar monitoring revealed that her fasting blood glucose levels steadily dropped and stabilized below 100 mg/dL. “It wasn’t just about the numbers,” she explains. “I felt healthier, more vibrant, and more in control of my life. The low GI approach changed everything.”
B. Testimonial: Michael’s Battle Against Diabetes
Michael, a 52-year-old man who had been battling diabetes for over a decade, found that his conventional diet and medications were not enough to keep his blood sugar in check. Desperate for a solution, he explored the low GI diet and was amazed by the results. “I started noticing improvements within just a few weeks,” Michael says. “I was less hungry, my energy levels improved, and most importantly, my blood sugar readings became much more stable.”
Michael’s journey was not without challenges. He had to overcome a long-standing habit of consuming high GI foods, but with determination and support from his family, he made the transition. “The key was to focus on quality over quantity,” he advises. Today, Michael’s blood sugar is well-controlled, and he credits his success to the simplicity and effectiveness of the low GI method.
C. Expert Insights: What Nutritionists Say
Nutrition experts are increasingly endorsing the low glycemic index diet as an effective tool for managing blood sugar levels. Dr. Emily Carter, a renowned endocrinologist, notes, “For many diabetics, a low GI diet can be a game‑changer. By focusing on foods that are slowly digested and absorbed, patients can avoid the sharp spikes in blood sugar that often lead to long-term complications.”
Dr. Carter adds that while a low GI diet is not a cure for diabetes, it is a powerful adjunct to conventional treatments. “The key is consistency and balance. Patients must combine dietary changes with regular exercise, medication when necessary, and ongoing monitoring. The low GI approach empowers patients to take control of their health in a very tangible way.”
IX. The Science of Glycemic Control: How It Works in Your Body
A. Digestion and Absorption: The Role of Low GI Foods
When you consume carbohydrates, your body breaks them down into glucose, which is then absorbed into the bloodstream. High GI foods are rapidly digested, leading to a swift surge in blood sugar levels. In contrast, low GI foods are digested more slowly due to their fiber content and complex carbohydrate structures. This slower digestion means that glucose is released gradually, leading to a more stable and controlled rise in blood sugar.
B. The Hormonal Response: Insulin and Glucose Regulation
Insulin is the hormone responsible for regulating blood sugar levels. When blood glucose levels rise rapidly, the pancreas releases a large amount of insulin to help cells absorb the sugar. This sudden surge can lead to a rapid drop in blood sugar later—a rollercoaster effect that can be particularly harmful for diabetics.
Low GI foods help modulate this hormonal response by ensuring that glucose enters the bloodstream at a steadier pace. This not only reduces the immediate demand for insulin but also helps prevent the sharp fluctuations that can damage cells over time. The result is improved insulin sensitivity and a lower risk of developing complications associated with diabetes.
C. The Long-Term Benefits of Stable Blood Sugar
Maintaining a blood sugar level below 100 mg/dL, particularly when fasting, is an important goal for many diabetics. Stable blood sugar levels contribute to:
-
Reduced Inflammation: Chronic high blood sugar is linked to systemic inflammation, which can exacerbate conditions like cardiovascular disease.
-
Better Energy Levels: Consistent blood sugar levels mean fewer energy crashes, leading to improved overall vitality.
-
Improved Metabolic Health: Stable glucose levels support healthy metabolic function, reducing the risk of complications such as neuropathy, kidney damage, and vision problems.
-
Enhanced Quality of Life: Ultimately, the goal is to help individuals live healthier, more active lives with fewer disruptions from blood sugar-related issues.
X. Integrating the Low GI Method Into Your Lifestyle
A. Building a Supportive Environment
Changing your diet can be challenging, especially when your current eating habits are deeply ingrained. One of the most effective ways to make a lasting change is to build a supportive environment. This might include:
-
Family and Friends: Encourage loved ones to join you in your journey. When those around you adopt healthier habits, it’s easier to stay motivated.
-
Online Communities: Join forums, social media groups, or local support groups focused on low GI eating and diabetes management. Sharing experiences, recipes, and tips can be incredibly empowering.
-
Professional Guidance: Work with a nutritionist or dietitian who specializes in diabetes management. Personalized advice can help tailor a low GI plan to your unique needs.
B. Practical Tools for Daily Success
Implementing a low GI diet is easier when you have the right tools:
-
Meal Planning Apps: Use digital tools to plan your meals, track your nutritional intake, and monitor your blood sugar levels.
-
Cookbooks and Recipes: Invest in cookbooks focused on low GI recipes or explore online resources to discover new dishes that are both delicious and healthy.
-
Food Journals: Keeping a food diary can help you track your progress, identify patterns, and stay accountable to your goals.
C. Overcoming Setbacks and Staying Consistent
Transitioning to a low GI diet may come with challenges. You might face setbacks, such as cravings for high GI foods or social situations where healthy options are limited. Here are some strategies to help you stay on track:
-
Plan Ahead: Always have low GI snacks on hand, and plan your meals in advance to avoid impulsive decisions.
-
Stay Flexible: It’s important to be flexible and understand that perfection is not the goal—consistency is. Allow yourself some leeway on occasion while maintaining your overall focus.
-
Celebrate Success: Recognize and celebrate your progress, no matter how small. Whether it’s an improvement in your blood sugar readings or simply feeling more energetic, every step forward is worth acknowledging.
XI. Success Stories: Real Lives Transformed by the Low GI Approach
A. Inspiring Journeys from Diabetics
Many individuals have experienced transformative benefits from adopting a low GI diet. Here are a few success stories that highlight the potential of this simple method:
1. Emma’s Transformation
Emma, a 38-year-old teacher, had struggled with Type 2 diabetes for years. Plagued by fatigue, frequent blood sugar spikes, and the frustration of managing her condition, she turned to a low GI diet as a last resort. “I was desperate to find a way to control my blood sugar without relying solely on medications,” Emma recalls. With the guidance of a nutritionist, Emma overhauled her eating habits—eliminating refined carbohydrates and incorporating more whole grains, fruits, and vegetables into her diet. Within a few months, her fasting blood sugar consistently dropped below 100 mg/dL, and she experienced a newfound energy and optimism that changed her outlook on life.
2. James’ Journey to Better Health
James, a 55-year-old former athlete, was diagnosed with diabetes after years of ignoring warning signs. Determined to reclaim his health, he adopted a low GI diet and complemented it with regular physical activity. “It wasn’t just about cutting carbs—it was about choosing the right kinds of carbs,” James explains. By focusing on low GI foods, he not only stabilized his blood sugar but also improved his overall fitness and mood. Today, James is an advocate for healthy eating and regularly shares his journey on social media to inspire others.
B. Expert Perspectives on Long-Term Benefits
Nutrition experts are increasingly recognizing the long-term benefits of a low GI diet for diabetes management. Dr. Karen Liu, an endocrinologist specializing in diabetes care, emphasizes, “The low glycemic index approach is not a fad—it’s based on solid science. By choosing foods that cause a gradual rise in blood sugar, patients can significantly reduce the burden on their pancreas and maintain better overall health.” Dr. Liu notes that while medications and exercise are important, diet is a cornerstone of effective diabetes management. “The method is simple, yet its impact can be profound when implemented consistently over time.”
C. How Success Stories Inspire Others
Success stories like those of Emma and James serve as powerful testimonials that a low GI diet can be a viable, sustainable method for keeping blood sugar under control. These narratives not only provide hope for those struggling with diabetes but also offer practical insights into how others can implement similar changes in their lives. By sharing these stories, communities of diabetics around the world are building support networks that foster motivation and encourage ongoing commitment to healthier eating habits.
XII. Addressing Challenges and Potential Pitfalls
A. Recognizing Individual Differences
It’s important to note that while a low GI diet can be highly effective for many people, it is not a one-size‑fits‑all solution. Each person’s body responds differently to various foods, and factors such as age, activity level, and overall health can influence blood sugar levels. What works well for one person might not be as effective for another. Therefore, it’s crucial to monitor your body’s responses and adjust your dietary plan accordingly.
B. Integrating With Other Diabetes Management Strategies
A low GI diet is a valuable tool in the management of diabetes, but it should be part of a comprehensive approach that includes:
-
Regular Exercise: Physical activity helps lower blood sugar by increasing insulin sensitivity and facilitating the uptake of glucose by muscle cells.
-
Medication Adherence: For many diabetics, medications are necessary to control blood sugar. Combining these with a low GI diet can lead to even better outcomes.
-
Stress Management: Stress can significantly affect blood sugar levels. Incorporating techniques such as mindfulness, yoga, or meditation can help maintain balance.
-
Regular Monitoring: Using a continuous glucose monitor (CGM) or keeping a detailed log of blood sugar readings can help you see the impact of dietary changes in real time.
C. Potential Obstacles and How to Overcome Them
Adopting a new diet is rarely without its challenges. Some common obstacles include:
-
Cravings for High GI Foods: It’s natural to crave familiar, high-energy foods, especially in moments of stress or fatigue. Plan for these moments by having healthy, low GI snacks available.
-
Social Situations: Eating out or attending social events can make sticking to a low GI diet challenging. Research menus in advance or suggest venues that offer healthier options.
-
Time Constraints: Meal planning and preparation require time and effort. Consider meal prepping on weekends or using convenient recipes that align with low GI principles.
Remember, the key is to stay consistent and be patient with yourself. Small, gradual changes often lead to lasting results.
XIII. The Future of Diabetes Management: Beyond Diet
A. Innovations in Glucose Monitoring
Advancements in technology are revolutionizing diabetes management. Continuous glucose monitors (CGMs) allow patients to track their blood sugar levels in real time, providing immediate feedback on how their dietary choices affect their glucose. These devices can be a game‑changer for those following a low GI diet, as they offer concrete data that can help fine‑tune food choices and meal timings.
B. Personalized Nutrition and Genetic Insights
As research in personalized medicine continues to grow, the future of diabetes management may include customized nutrition plans based on individual genetic profiles. Understanding how your unique genetic makeup influences your metabolism and response to different types of carbohydrates can lead to more effective, tailored dietary strategies.
C. Integrative Approaches to Health
Modern diabetes management is increasingly integrative, combining dietary changes with physical activity, medication, and behavioral therapy. This holistic approach addresses not just blood sugar control but overall quality of life. Innovations in telemedicine and digital health apps are making it easier than ever for patients to access support, track their progress, and make informed decisions about their health.
XIV. The Role of Education and Empowerment
A. Empowering Yourself Through Knowledge
Knowledge is power, especially when it comes to managing a chronic condition like diabetes. Understanding the glycemic index, learning about how different foods affect your blood sugar, and staying informed about the latest research can empower you to take control of your health. Educational resources—such as books, online courses, and support groups—can provide valuable insights and practical advice for living a healthier life.
B. Building a Support Network
Managing diabetes is a journey best undertaken with support. Whether it’s joining a local diabetes support group or connecting with others online, sharing your experiences and learning from others can make a significant difference. These networks not only offer emotional support but also practical tips and encouragement to stay on track with your low GI diet and other health goals.
C. Advocating for Better Healthcare
By educating yourself and others about effective diabetes management strategies, you can become an advocate for better healthcare policies. Sharing success stories, participating in community outreach, and engaging with healthcare professionals can help drive improvements in diabetes care and education. Empowerment begins with awareness—and by spreading knowledge, you contribute to a broader movement toward healthier, more informed communities.
XV. Real-Life Experiences: Voices of Those Who Have Made the Change
A. Inspirational Testimonials
Throughout this article, we’ve highlighted the journeys of individuals like Emma and James, whose lives have been transformed by adopting a low GI diet. Their stories are not isolated cases but part of a growing body of evidence that shows how simple dietary adjustments can lead to significant improvements in health. For many diabetics, these testimonials serve as a beacon of hope—a reminder that managing blood sugar is achievable and that better health is within reach.
B. The Ripple Effect of Positive Change
When one person takes charge of their health, it can have a ripple effect on those around them. Friends, family members, and even healthcare providers are inspired by the success of individuals who embrace a low GI diet. As more people adopt this approach, the collective impact can lead to broader improvements in public health, reduced healthcare costs, and a higher quality of life for diabetics everywhere.
C. Lessons Learned and Tips for Success
Success in managing diabetes is often a series of small victories. Here are some key lessons and tips from those who have successfully implemented a low GI diet:
-
Plan Ahead: Consistent meal planning can prevent impulsive decisions that might lead to high blood sugar spikes.
-
Stay Educated: Keep up with the latest research and dietary recommendations to refine your approach.
-
Monitor Progress: Use tools like CGMs and food diaries to track how your body responds to different foods.
-
Seek Professional Guidance: A nutritionist or dietitian specialized in diabetes can provide personalized advice and support.
-
Celebrate Milestones: Recognize your progress and the positive changes in your health. Every improvement is a step toward a better quality of life.
XVI. The Science in Action: Integrating Research With Daily Practice
A. Translating Research Into Real‑World Benefits
The benefits of a low GI diet for diabetics are not just theoretical—they are backed by extensive scientific research. Studies consistently show that individuals who adopt a low GI dietary approach experience improved glycemic control, reduced insulin resistance, and enhanced overall metabolic health. These benefits translate into tangible improvements in daily life: more stable energy levels, better mood, and a lower risk of complications such as heart disease and neuropathy.
B. Case Studies and Clinical Trials
Numerous clinical trials have examined the impact of low GI diets on diabetics. For example, a randomized controlled trial published in Diabetes Care found that participants following a low GI diet had significantly lower postprandial (after-meal) blood sugar levels compared to those on a conventional diet. Other studies have reported improvements in HbA1c levels—a key marker of long‑term blood sugar control—among patients who switched to low GI foods.
These case studies underscore that the method is not only simple but also effective. By integrating these findings into daily practice, diabetics can achieve better blood sugar control and reduce the burden of managing their condition. Healthcare providers are increasingly recommending low GI diets as part of a comprehensive diabetes management plan, reinforcing the idea that simple, well-informed choices can lead to profound health benefits.
C. The Role of Continuous Monitoring
Advancements in technology, such as continuous glucose monitoring (CGM), have made it easier than ever to see the immediate effects of dietary changes. CGMs provide real‑time data on blood sugar levels, allowing patients to adjust their diets based on concrete evidence. For diabetics following a low GI diet, this technology serves as both a motivator and a feedback tool. Watching the direct impact of their food choices on blood sugar levels can reinforce positive habits and help patients fine‑tune their diets for optimal results.
XVII. The Future of Diabetes Management: Integrative Approaches and New Technologies
A. Personalized Nutrition
The future of diabetes management lies in personalized nutrition. As genetic research and personalized medicine continue to evolve, diabetics may soon receive tailored dietary recommendations based on their unique metabolic profiles. A personalized low GI plan could optimize blood sugar control even further, taking into account individual differences in digestion, metabolism, and lifestyle.
B. Digital Health and Data Integration
Digital health technologies are rapidly transforming how we manage chronic conditions. Smartphone apps that track food intake, blood sugar levels, physical activity, and medication adherence are becoming essential tools for diabetics. The integration of these digital tools with a low GI dietary approach offers a holistic view of health, enabling patients to make data‑driven decisions and adjust their lifestyle in real time. As these technologies advance, they will play an increasingly important role in helping diabetics maintain stable blood sugar levels and achieve overall wellness.
C. A Holistic Approach to Health
A low GI diet is just one piece of the puzzle. Effective diabetes management involves a holistic approach that includes physical activity, stress management, adequate sleep, and regular medical checkups. Future strategies will likely focus on integrating these various aspects of health into a comprehensive management plan that addresses not only blood sugar control but also overall well‑being. As research continues to uncover the complex interplay between diet, lifestyle, and metabolic health, a more integrative approach will emerge—one that empowers individuals to take full control of their health.
XVIII. The Role of Education and Community Support
A. Empowering Diabetics Through Information
Education is a powerful tool in managing diabetes. By understanding the science behind blood sugar control and the benefits of a low GI diet, patients are better equipped to make informed decisions about their health. Educational resources—ranging from online articles and webinars to in‑person workshops and support groups—play a crucial role in empowering diabetics. Knowledge about how different foods affect blood sugar can transform daily habits and lead to lasting improvements in health.
B. Building a Supportive Community
The journey of managing diabetes can be isolating, but it doesn’t have to be. Connecting with others who are on the same path can provide emotional support, practical tips, and a sense of camaraderie. Whether it’s joining a local diabetes support group or participating in online forums and social media communities, sharing experiences and strategies can make a significant difference. Community support helps reinforce the importance of sticking to a low GI diet, especially during challenging times, and fosters a collective commitment to better health.
C. Advocating for Better Healthcare Policies
As more individuals experience the benefits of a low GI diet, there is an opportunity to advocate for broader changes in healthcare policy. Public awareness of effective, simple methods for managing diabetes can drive policy changes that promote nutritional education, support for dietary programs, and research into personalized medicine. By sharing success stories and data on the effectiveness of low GI diets, diabetics and healthcare professionals can work together to influence policy and improve healthcare outcomes on a larger scale.

XIX. Integrating the Low GI Diet With Lifestyle Changes
A. Combining Diet With Regular Exercise
While diet is a crucial factor in managing blood sugar, it works best when combined with regular physical activity. Exercise helps improve insulin sensitivity, reduce body fat, and maintain a healthy weight—all of which contribute to more stable blood sugar levels. A holistic approach that integrates a low GI diet with consistent exercise routines can have a synergistic effect, leading to better overall metabolic health.
B. Stress Management and Its Impact on Blood Sugar
Stress is another critical factor that can influence blood sugar levels. Chronic stress triggers the release of cortisol, a hormone that can lead to increased blood sugar and insulin resistance. Incorporating stress management techniques—such as mindfulness, meditation, yoga, or even simple breathing exercises—can complement a low GI diet by helping to regulate hormonal responses and reduce the risk of blood sugar spikes.
C. The Importance of Sleep and Recovery
Adequate sleep is essential for maintaining overall health and supporting metabolic processes. Poor sleep can lead to elevated blood sugar levels and contribute to insulin resistance. By prioritizing good sleep hygiene and ensuring that you get enough rest, you can enhance the effectiveness of a low GI diet and contribute to better long‑term blood sugar control.
XX. Monitoring Your Progress: Tools and Techniques
A. Using Continuous Glucose Monitors
Continuous glucose monitors (CGMs) have revolutionized diabetes management by providing real‑time data on blood sugar levels. For those following a low GI diet, CGMs offer immediate feedback on how specific foods and meals affect their glucose levels. This data can be invaluable in fine‑tuning your dietary choices and ensuring that you consistently maintain blood sugar levels below 100 mg/dL.
B. Keeping a Food and Symptom Diary
A food diary is a practical tool that helps you track your dietary habits and monitor the effects on your blood sugar. Recording what you eat, along with your blood sugar readings and any symptoms you experience, can reveal patterns and identify which foods work best for you. Over time, this diary can become an essential part of your diabetes management toolkit, allowing you to make data‑driven decisions about your diet.
C. Regular Consultations With Healthcare Providers
While self‑monitoring is important, regular consultations with your healthcare provider are crucial for effective diabetes management. Your doctor can help interpret your blood sugar data, adjust medications if needed, and provide guidance on integrating a low GI diet into your overall treatment plan. Routine checkups and blood tests—such as HbA1c measurements—ensure that you are on track and that any necessary adjustments are made promptly.
XXI. The Long-Term Benefits of Keeping Your Blood Sugar Below 100
A. Reduced Risk of Complications
Maintaining fasting blood sugar levels below 100 mg/dL can significantly reduce the risk of long‑term complications associated with diabetes. Chronic high blood sugar is linked to a host of health problems, including heart disease, kidney failure, nerve damage, and vision loss. By keeping your blood sugar in check, you are taking proactive steps to protect your health and prevent these potentially debilitating conditions.
B. Improved Energy and Quality of Life
Stable blood sugar levels lead to more consistent energy throughout the day. When your body isn’t constantly grappling with spikes and crashes, you’ll experience improved stamina, mental clarity, and overall vitality. This, in turn, enhances your quality of life, allowing you to engage more fully in daily activities and pursue your passions without being held back by fatigue or health complications.
C. Enhanced Metabolic Health and Weight Management
A low GI diet not only helps regulate blood sugar but also supports healthy metabolism and weight management. By preventing rapid insulin spikes and controlling hunger, this approach can help you maintain a healthy weight—a crucial factor in managing diabetes. A balanced, nutrient‑rich diet combined with regular exercise can lead to improved metabolic function and a reduced risk of obesity-related complications.
XXII. Common Questions and Concerns About the Low GI Method
A. Is the Low GI Diet Suitable for Everyone?
While a low GI diet can be highly beneficial for many diabetics, it is important to remember that every individual is unique. Factors such as age, activity level, other health conditions, and personal preferences play a role in determining the best dietary approach. It is advisable to consult with a healthcare provider or nutritionist before making significant dietary changes.
B. How Do I Know If I’m Making the Right Choices?
Monitoring your blood sugar levels is key. Using tools like CGMs and maintaining a food diary can help you see the direct impact of your dietary choices. Over time, you’ll learn which foods work best for your body and which ones may cause undesirable spikes in blood sugar.
C. Can I Still Enjoy My Favorite Foods?
Absolutely. The goal of a low GI diet is not to eliminate pleasure from eating but to make smarter choices. With a bit of creativity and planning, you can enjoy many of your favorite meals while still keeping your blood sugar in check. Moderation and substitution are the keys to balancing indulgence with health.
D. What If I Experience Setbacks?
It’s important to remember that managing diabetes is a journey, not a destination. There may be times when your blood sugar levels aren’t where you want them to be. In those instances, review your food diary, adjust your meal plan if needed, and consult with your healthcare provider. Small setbacks are part of the process, and persistence is key to long‑term success.
XXIII. Expert Opinions and Clinical Evidence
A. What Do Nutritionists Say?
Many nutritionists and endocrinologists advocate for the low GI diet as an effective tool for managing diabetes. Dr. Lisa Nguyen, a specialist in metabolic disorders, emphasizes, “A low glycemic index diet helps smooth out the peaks and valleys of blood sugar levels. It’s a simple, natural approach that works in concert with your body’s own regulatory mechanisms.” Dr. Nguyen adds that when combined with other lifestyle modifications, such as exercise and stress management, the low GI approach can significantly improve overall health and reduce the risk of diabetes complications.
B. Clinical Trials and Research Findings
Clinical trials consistently show that patients who follow a low GI diet experience better glycemic control and improved metabolic markers. For example, a study published in Diabetes Care found that participants on a low GI diet had lower postprandial blood glucose levels and improved HbA1c scores compared to those on a conventional diet. These findings are supported by numerous other studies, making the low GI method a well‑established approach in the field of diabetes management.
C. Long-Term Outcomes and Patient Testimonials
Over the years, many patients have reported remarkable improvements in their health after adopting a low GI diet. These testimonials, backed by clinical evidence, offer a compelling case for the method. Patients report not only better blood sugar control but also enhanced energy levels, improved mood, and a better quality of life. Such success stories underscore the potential of the low GI diet to transform lives and provide a blueprint for effective, sustainable diabetes management.
XXIV. Integrating a Low GI Diet Into a Comprehensive Diabetes Management Plan
A. Diet, Exercise, and Medication: A Holistic Approach
Effective diabetes management is multifaceted. A low GI diet is a critical component, but it works best when integrated with other lifestyle modifications such as regular physical activity and adherence to prescribed medications. Exercise helps increase insulin sensitivity and further stabilizes blood sugar levels, while medications can assist in maintaining the delicate balance needed for optimal health. The synergy between these elements—diet, exercise, and medication—creates a robust framework for managing diabetes and preventing complications.
B. Personalizing Your Diabetes Plan
No two individuals are the same, and personalizing your diabetes management plan is essential. Work with your healthcare provider to tailor a plan that fits your lifestyle, preferences, and medical needs. This may include:
-
Regular Monitoring: Using tools like CGMs to track your blood sugar in real time.
-
Dietary Adjustments: Experimenting with different low GI foods and recipes to find what works best for you.
-
Exercise Routines: Incorporating physical activities that you enjoy, whether it’s walking, cycling, or swimming.
-
Stress Management Techniques: Adopting practices such as meditation, yoga, or deep breathing to help control stress, which can impact blood sugar levels.
C. Overcoming Barriers and Building Resilience
Challenges are inevitable in any health journey, but they can be overcome with the right mindset and support system. Identify potential barriers—be they social, emotional, or logistical—and work proactively to address them. Whether it’s finding low GI options when eating out or managing cravings for high GI foods, small adjustments can make a big difference. Building resilience through community support, education, and consistent self-monitoring will empower you to maintain your health and stay on track.
XXV. Conclusion: A Simple Method with Profound Impact
Diabetes is a complex condition that requires a multifaceted approach to management. Among the various strategies available, adopting a low glycemic index diet stands out as one simple, effective method to keep your blood sugar levels below 100 mg/dL. By focusing on the quality of carbohydrates, emphasizing high-fiber and nutrient-dense foods, and integrating this approach with regular exercise and proactive monitoring, you can create a dietary environment that supports stable blood sugar levels and overall well-being.
This comprehensive article has explored 15 warning signs of cancer and, more importantly, provided an in-depth guide on how a low GI diet can be a game-changer for diabetics. The method is straightforward, grounded in solid scientific principles, and supported by both clinical evidence and real-life success stories. Early detection and consistent management are key to preventing complications and living a vibrant, healthy life.
Remember, managing diabetes is a journey that requires commitment, support, and the willingness to make small, sustainable changes every day. By taking control of your diet and making informed choices, you empower yourself to live better and healthier—one meal at a time.
If you have concerns about your blood sugar levels or need guidance on adopting a low GI diet, please consult a healthcare provider or a nutrition expert who can help tailor this approach to your unique needs. Your health is your most valuable asset, and taking these steps today can lead to a brighter, healthier future.
Meta Description:
Learn how a low glycemic index diet can help diabetics keep blood sugar levels below 100 mg/dL. This comprehensive guide (over 6,000 words) covers the science behind low GI foods, practical meal planning tips, success stories, and the long-term benefits of stabilizing blood sugar.